10 Tips to Reduce Medical Billing Claim Denials
Medical billing claim denials are one of the most significant obstacles healthcare providers face when it comes to maintaining a healthy cash flow. The consequences of these denials can lead to delayed payments, increased administrative burdens, and a substantial loss of revenue. Reducing claim denials should be a priority for any medical practice seeking to optimize its revenue cycle management (RCM).

With the complexity of medical billing regulations and insurance requirements, even the most meticulous practices can experience claim rejections. However, by adopting best practices, leveraging advanced technology, and incorporating strategic denial management solutions, healthcare providers can dramatically reduce the likelihood of claim denials and improve overall financial performance.
Actionable Tips for Smoother Medical Billing Claims Process
1. Verify Insurance Eligibility and Coverage Early
Insurance verification at the point of registration is the first line of defense against claim denials. Ensure that all patient insurance details—such as eligibility, coverage, and policy limits—are verified before services are rendered. Confirming this information reduces the risk of claims being denied due to incorrect or outdated insurance data. CapitalMed Solutions provides robust insurance verification services to ensure that your claims have the highest chance of acceptance.
2. Ensure Accurate Medical Coding
Coding errors, such as upcoding, undercoding, or outdated codes, are some of the most common causes of denied claims. It is essential to ensure that medical codes align precisely with the diagnoses and services provided. By staying current with the latest ICD-10, CPT, and HCPCS coding guidelines, your practice can minimize errors and improve reimbursement rates. Partnering with CapitalMed Solutions’ certified coding experts guarantees compliance and accuracy in every claim submission.
3. Submit Complete and Clean Claims
A “clean claim” is one that contains all the necessary details without errors or omissions. Incomplete or incorrect claims often result in denials or delays in payment. Before submitting claims, ensure they are thoroughly reviewed for completeness. This includes accurate patient information, valid diagnosis codes, and appropriate procedural codes. Implementing a system to track and review claims will further reduce the chance of submission errors.
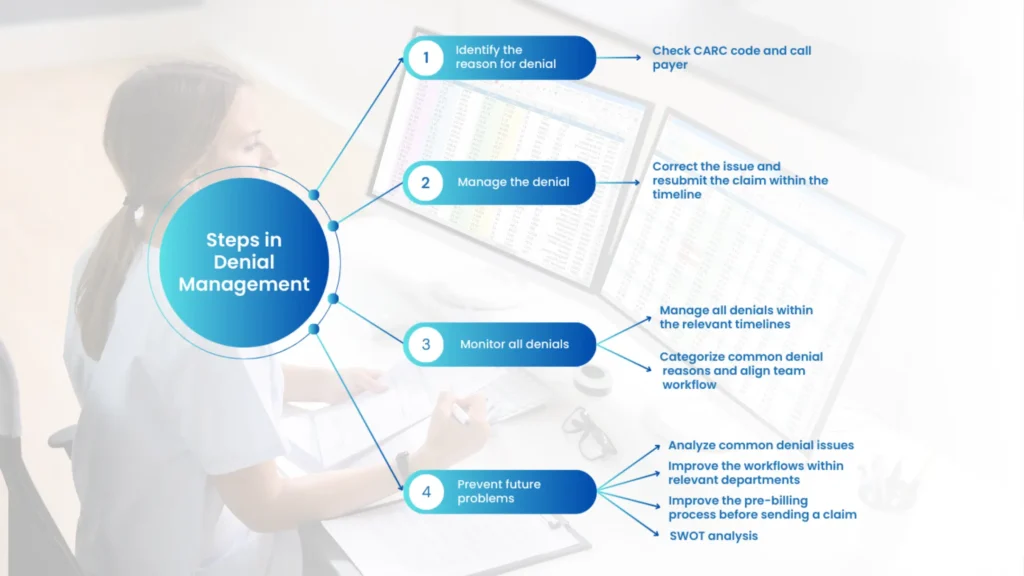
4. Monitor Denial Trends and Root Causes
Understanding the reasons behind claim denials is crucial to addressing recurring issues. Regularly tracking denial trends and analyzing root causes allows your practice to identify and correct systemic problems. Whether it’s coding discrepancies, missing authorizations, or eligibility issues, monitoring denials will help you proactively mitigate these problems in the future. At CapitalMed Solutions, our advanced analytics help healthcare providers track and resolve denial patterns effectively.
5. Implement a Timely Denial Appeal Process
The faster your team responds to denied claims, the higher the likelihood of recovery. Establishing a streamlined process for denial management—including the timely resubmission of claims and appeals—can help recover lost revenue. Delaying the appeal process can result in missed reimbursement opportunities. CapitalMed Solutions provides dedicated denial management services to ensure that no revenue is left on the table.
6. Leverage EHRs and Practice Management Software
Utilizing Electronic Health Records (EHRs) and comprehensive practice management software is a highly effective way to streamline billing processes and improve accuracy. These systems automate key functions such as eligibility verification, claim submissions, and follow-ups, reducing manual errors and speeding up the reimbursement process. Automation minimizes human errors and improves the overall efficiency of your practice’s revenue cycle management.
7. Invest in Continuous Staff Training
Medical billing and coding are complex and continually evolving fields. Regular training for your billing and administrative team ensures that they stay informed about the latest industry standards, payer policies, and coding updates. Well-trained staff are less likely to make costly mistakes and are better equipped to resolve issues quickly. At CapitalMed Solutions, we provide ongoing training for your team to ensure they remain at the forefront of the industry.
8. Maintain Thorough and Accurate Documentation
Detailed and accurate documentation is essential for supporting claims. Insufficient or vague documentation can lead to claim denials, especially when insurance companies require proof of medical necessity. Ensure that each patient’s visit is properly documented with clear, concise descriptions of services rendered. This documentation serves as the foundation for your claims, allowing you to justify the procedures and treatments billed.
9. Ensure Proper Authorization for Services
Many medical procedures and services require prior authorization from insurance providers. Failing to obtain authorization beforehand can result in a denial of claims. By staying proactive and checking for authorization requirements before services are provided, you can avoid delays and ensure the timely reimbursement of claims. Proper authorization ensures that your practice remains compliant and reduces the risk of denials for these services.
10. Outsource Medical Billing to Experts
Managing the entire revenue cycle in-house can become overwhelming, especially as your practice grows. Outsourcing medical billing to a trusted partner like CapitalMed Solutions allows you to focus on patient care while experts handle the complexities of medical billing and revenue cycle management. Our team provides comprehensive, end-to-end RCM services, from coding and billing to denial management and payment posting, ensuring maximum revenue recovery and minimal claim denials.
Conclusion
Reducing medical billing claim denials requires a comprehensive, proactive approach. By verifying insurance details, ensuring accurate coding, leveraging automation, training staff, and implementing efficient denial management strategies, healthcare providers can significantly reduce the frequency of claim rejections. Partnering with a trusted Revenue Cycle Management provider like CapitalMed Solutions can further streamline these efforts, providing your practice with the expertise and support needed to optimize its financial performance.
With a strategic approach to billing and a focus on continuous improvement, your practice can minimize claim denials, improve cash flow, and ultimately enhance profitability.