Streamline Your Practice Onboarding with CapitalMed Solutions
Provider Enrollment and Credentialing Services
At CapitalMed Solutions, we understand that provider enrollment and credentialing are crucial components of healthcare practice management. Our specialized provider enrollment and credentialing services ensure that healthcare providers meet regulatory standards and are properly enrolled with insurance plans, enabling them to deliver quality care while maximizing revenue through efficient provider enrollment & credentialing processes.

Why Choose CapitalMed Solutions for Provider Enrollment and Credentialing?
When you partner with CapitalMed Solutions, a proven medical billing company, you gain specialized credentialing and enrollment services tailored to your practice. We handle everything from application to re-credentialing, accelerating your revenue cycle from day one.
Experienced Credentialing Professionals: Our team comprises experts with extensive knowledge of healthcare provider enrollment and credentialing requirements across all major payers.
Customized Enrollment Solutions: We tailor our provider enrollment and credentialing services to fit the specific needs of your practice, regardless of its size or specialty.
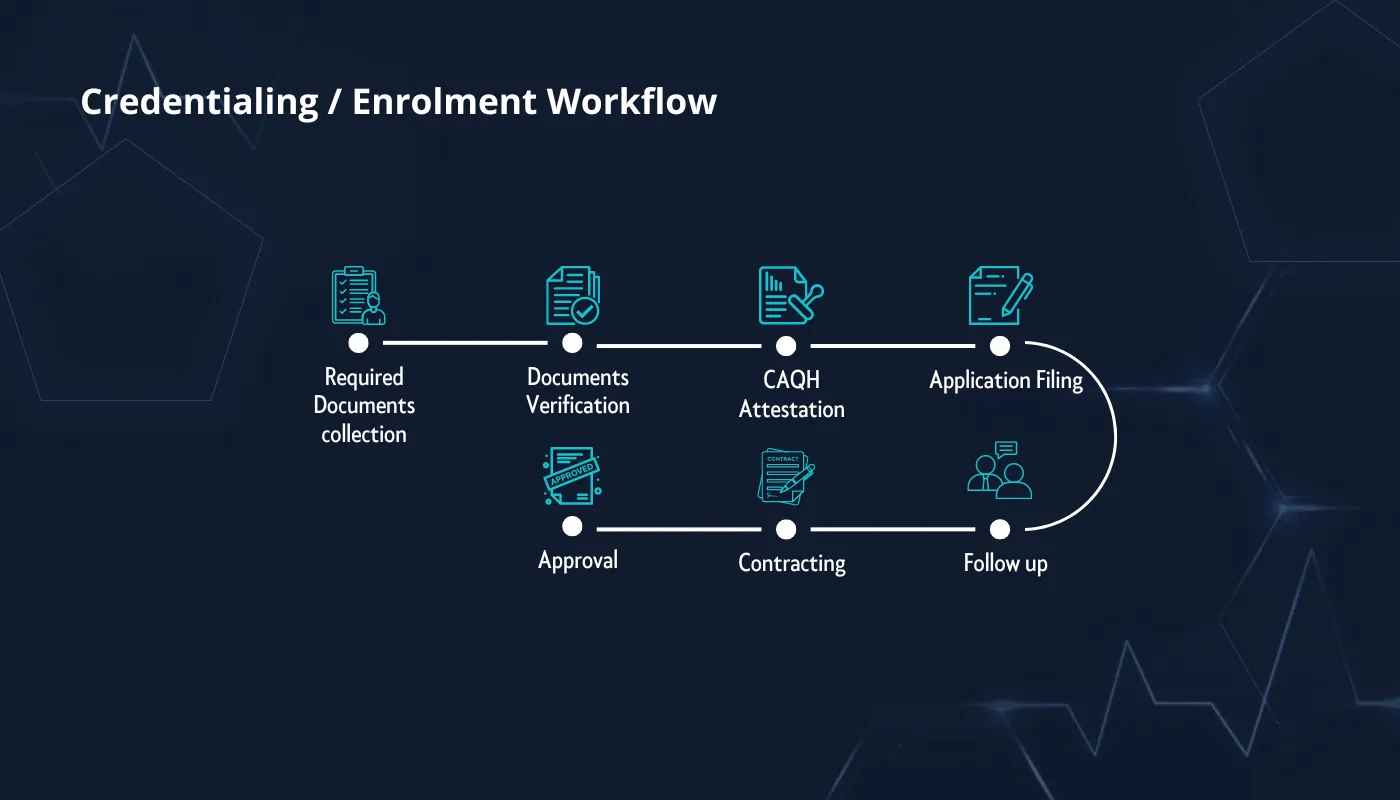
Comprehensive Enrollment Support: Our dedicated team guides you through every step of the provider enrollment & credentialing process from start to finish.
Focus on Compliance: We ensure all credentialing and enrollment processes adhere to industry standards and regulations, minimizing the risk of audits and penalties.
States We Serve for Provider Enrollment and Credentialing Services
PROVIDER ENROLLMENT AND CREDENTIALING SERVICES
At CapitalMed Solutions, we offer expert provider enrollment and credentialing services to help healthcare providers navigate the complex process of becoming credentialed with insurance payers. Our dedicated team ensures that all required documentation for provider enrollment and credentialing services is accurately prepared and submitted, reducing delays and rejections.
By streamlining provider enrollment & credentialing for individual providers or entire practices, we help you gain quicker access to reimbursements, allowing your practice to focus on delivering quality patient care while expanding your patient base through efficient credentialing and enrollment management.
EDI/ERA/EFT Setup
CAQH Attestation
NPI Registration
Revalidation
Government payers Credentialing/Enrollment
Hospital Appointments
Commercial Payers Credentialing/Enrollment
Contract Negotiation
Benefits of Provider Enrollment and Credentialing Services
Getting professional provider enrollment and credentialing services from CapitalMed Solutions offers numerous benefits to your healthcare practice:
Improved Operational Efficiency
Streamlining the credentialing and enrollment process reduces administrative burdens on your staff.
Faster Reimbursement Access
Proper provider enrollment & credentialing ensures you can begin billing insurance payers quickly, accelerating your revenue cycle.
Reduced Administrative Burden
Our comprehensive credentialing and enrollment services free your staff from complex paperwork and follow-up tasks.
Specialty Billing and Coding Services We Offer
Individual Practices
Nursing Homes
Healthcare Systems
Skilled Nursing Facilities
Group Practices
Independent Labs
Hospitals
Surgical centers
Hospitalist Group
Home Health
Freestanding Emergency Rooms
Urgent care Centers
DME Suppliers
Rehab Centers
Freestanding Emergency Rooms
Acupuncture
DME
Emergency Rooms
ENT
Endocrinology
General Surgery
Dentistry
Hepatology
Home Health Services
Rheumatology
Surgery
Speech Therapy
Telemedicine
FAQs about Provider Enrollment and Credentialing
Interested to Learn More About Our Credentialing and Enrollment Services?
Lets Get In Touch
Working Hours
Monday – Friday 09 AM To 05 PM
Our Location
77 Sugarcreek Blvd Suite 600, Sugar land, TX 77478

