How to Optimize Your Medical Practice’s Revenue Cycle
In an increasingly complex healthcare environment, optimizing the revenue cycle is critical to maintaining the financial health of any medical practice. A well-managed revenue cycle improves cash flow, minimizes claim denials, and enhances the overall efficiency of your operations.

However, many providers face challenges due to administrative inefficiencies, inaccurate coding, and delays in collections. Understanding and refining each phase of the revenue cycle can lead to significant improvements in performance and profitability.
Understanding the Revenue Cycle
The medical revenue cycle encompasses every administrative and clinical function involved in capturing, managing, and collecting patient service revenue. This includes:
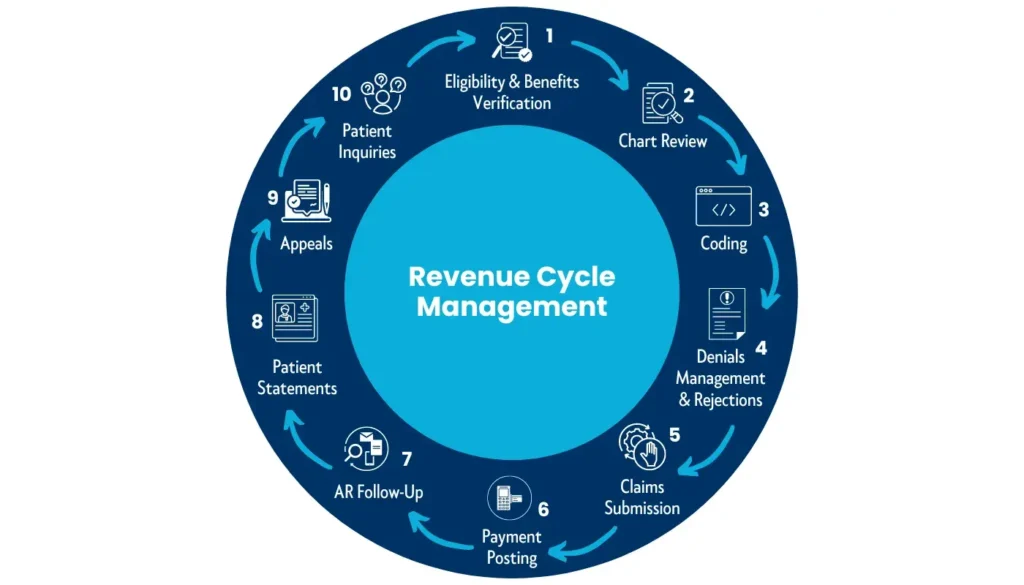
- Patient scheduling and insurance verification
- Documentation and coding
- Claims submission and processing
- Payment posting
- Denial resolution and collections
Even minor missteps at any stage can result in lost revenue or regulatory risks.
Enhance Front-End Accuracy
Revenue cycle optimization begins at the front desk. Inaccurate or incomplete patient data during registration can lead to downstream billing issues.
- Verify insurance eligibility prior to each visit
- Collect co-pays and outstanding balances at check-in
- Train staff on data entry accuracy and common registration errors
By ensuring clean data from the outset, practices can significantly reduce claim rejections.
Implement Precise Medical Coding
Accurate coding is foundational to successful revenue cycle management. Errors such as upcoding, undercoding, or outdated code usage can lead to payment delays, audits, or even penalties.
Leveraging the expertise of certified coders—such as those at CapitalMed Solutions—ensures compliance with the latest CPT, ICD-10, and HCPCS guidelines while maximizing reimbursement potential.
Embrace Automation and Technology
Revenue cycle optimization begins at the front desk. Inaccurate or incomplete patient data during registration can lead to downstream billing issues.
- Verify insurance eligibility prior to each visit
- Collect co-pays and outstanding balances at check-in
- Train staff on data entry accuracy and common registration errors
By ensuring clean data from the outset, practices can significantly reduce claim rejections.
Implement Precise Medical Coding
Accurate coding is foundational to successful revenue cycle management. Errors such as upcoding, undercoding, or outdated code usage can lead to payment delays, audits, or even penalties.
Leveraging the expertise of certified coders—such as those at CapitalMed Solutions—ensures compliance with the latest CPT, ICD-10, and HCPCS guidelines while maximizing reimbursement potential.
Embrace Automation and Technology
Manual processes not only consume valuable staff time but also increase the likelihood of errors. Implementing practice management systems, electronic health records (EHRs), and automated billing tools can lead to:
- Accelerated claims processing
- Enhanced data accuracy
- Improved patient communication and follow-up
Automation enables your team to focus more on patient care while optimizing administrative workflows.
Track Key Revenue Cycle Metrics
Monitoring the right performance indicators is essential to identifying inefficiencies and improving financial outcomes. Key metrics include:
- Days in Accounts Receivable (A/R)
- First-pass claim acceptance rate
- Net collection rate
- Denial rate
Consistent evaluation of these KPIs enables data-driven decision-making and continuous improvement.
Establish a Robust Denial Management Process
Claims denials represent one of the most common revenue drains for medical practices. A proactive denial management strategy should include:
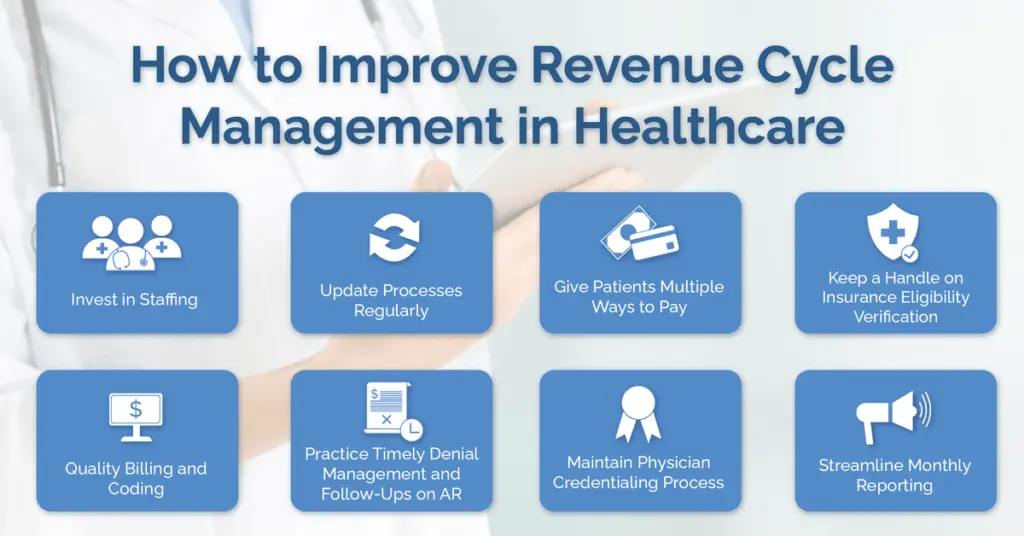
- Root cause analysis of common denials
- Timely appeals of eligible claims
- Systematic prevention of recurring issues
CapitalMed Solutions provides dedicated denial management support to recover lost revenue and reduce future denials.
Invest in Staff Training and Development
Your team plays a pivotal role in the success of your revenue cycle. Ongoing training ensures that staff remain current with payer policies, billing procedures, and compliance standards.
Empowered staff are better equipped to:
- Communicate effectively with patients regarding their financial responsibilities
- Minimize errors in charge capture and documentation
- Respond promptly to billing inquiries and payer communications
Consider Outsourcing Revenue Cycle Management
Managing a full-scale revenue cycle in-house can strain resources and limit scalability. Outsourcing to a trusted partner like CapitalMed Solutions can offer:
- Access to experienced billing and coding specialists
- Scalable services tailored to your practice’s growth
- Significant reductions in operational overhead
- Improved collections and regulatory compliance
CapitalMed Solutions delivers comprehensive, HIPAA-compliant RCM services that empower healthcare providers to focus on delivering exceptional patient care.
Conclusion
Optimizing the revenue cycle is not a one-time initiative—it’s an ongoing process that requires strategic planning, operational excellence, and a commitment to improvement. By enhancing front-end accuracy, leveraging technology, tracking performance metrics, and partnering with experienced professionals, your practice can drive better financial outcomes and long-term sustainability.
At CapitalMed Solutions, we help healthcare organizations overcome revenue challenges through customized, end-to-end revenue cycle management solutions. Let us help you take control of your revenue cycle—efficiently, compliantly, and profitably.