Denial Management Services in Florida
At CapitalMed Solutions, we specialize in providing efficient and results-driven denial management services in Florida to help healthcare providers recover lost revenue and prevent recurring claim denials. Our experienced billing specialists analyze, correct, and resubmit denied claims while identifying root causes to enhance future claim acceptance rates—keeping your revenue cycle strong and healthy.

Why Florida Providers Choose Our Denial Management Services
Comprehensive Denial Analysis: We perform in-depth audits to identify the causes of claim denials—whether due to missing documentation, incorrect coding, or payer-specific rules—ensuring accurate resolution every time.
Quick Rebilling and Recovery: Our denial management experts correct and resubmit claims within payer time limits to recover lost revenue swiftly, minimizing cash flow disruptions.
Root Cause Prevention: We don’t just fix denied claims; we prevent them. Our proactive tracking and analytics help practices reduce recurring errors, improving first-pass acceptance rates.
Local Florida Expertise: We understand payer policies and healthcare regulations specific to Florida. Our close coordination with insurance carriers helps accelerate denial resolution and compliance.
Our Denial Management Process in Florida
At CapitalMed Solutions, we use a structured, transparent process designed to minimize claim denials, accelerate reimbursements, and improve your overall revenue cycle performance. As a trusted Medical Billing Services Company in Florida, we partner with healthcare providers to streamline billing operations and enhance financial outcomes.
Denial Identification & Categorization
We identify denied claims from clearinghouses or payer remittances and categorize them (coding errors, eligibility issues, missing modifiers, etc.) for quick and accurate resolution.
Root Cause Analysis
Our team reviews EOBs and denial codes to determine the exact reason for each rejection. This helps us address the underlying issue and prevent it from happening again.
Claim Correction & Re-submission
We correct claim details—such as CPT/ICD codes, patient demographics, or insurance information—and resubmit them electronically for faster reimbursement.
Appeals Management
For denied claims requiring formal appeals, we prepare complete documentation and communicate directly with payers to ensure reconsideration and successful reimbursement.
Tracking & Reporting
We maintain detailed denial logs and generate reports highlighting denial types, payer trends, and resolution timelines—giving you full visibility into claim performance.
Prevention Strategy & Training
We work with your billing and front-office teams to identify process gaps, improve documentation practices, and implement system checks that prevent future denials.
Benefits of Choosing CapitalMed Solutions for Denial Management in Florida

Why CapitalMed Solutions Is the Trusted Denial Management Partner in Florida
At CapitalMed Solutions, we combine technology, expertise, and a proactive approach to ensure you recover every dollar you’ve earned. Our dedicated denial management team helps Florida practices of all sizes eliminate revenue leakage and improve reimbursement accuracy.
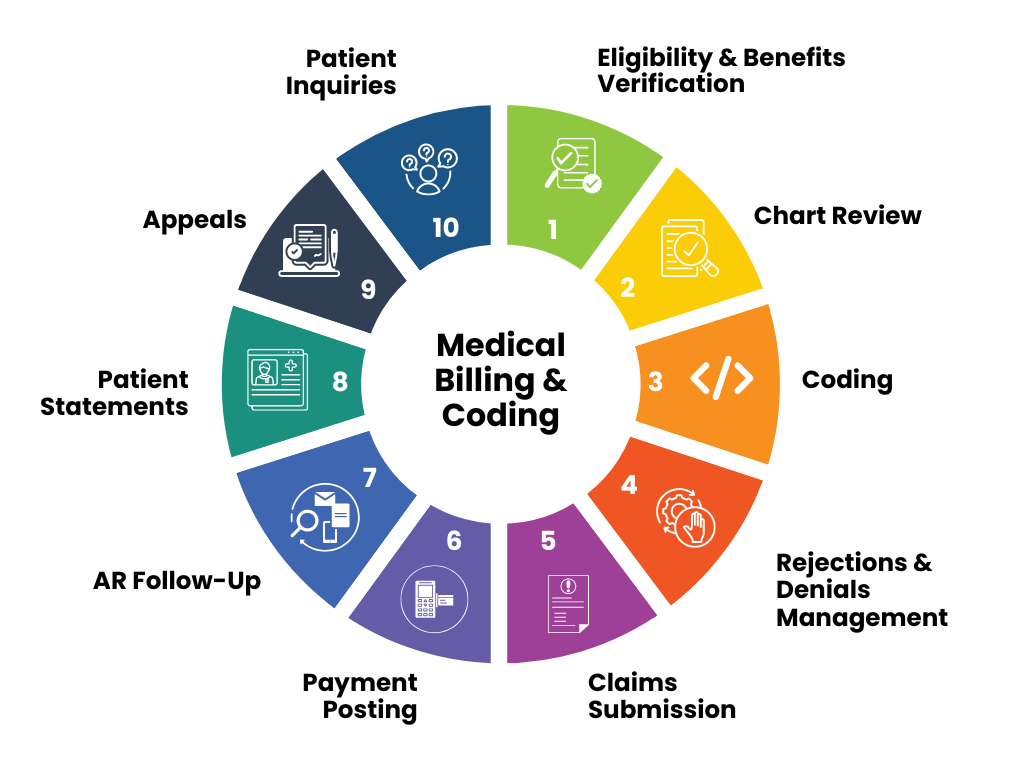
Our Denial Management Services Process in Florida
Our comprehensive Denial Management Services program ensures you receive the highest quality service
Ready to Simplify Denial Management in Florida?
Connect with our denial management specialists today to identify, fix, and prevent claim denials before they impact your cash flow. Let CapitalMed Solutions handle your denials—so you can focus on quality patient care.
Working Hours
Monday – Friday 09 AM To 05 PM
Our Location
77 Sugarcreek Blvd Suite 600, Sugar Land, TX 77478

